HIV infection
UNAIDS and the WHO estimate that in 20111:
- 34 million people worldwide were living with HIV
- 2.5 million people became newly-infected with HIV
- 1.7 million people died from AIDS-related illnesses
Definition
The human immunodeficiency virus (HIV) is a lentivirus (family of retroviruses) that targets white blood cells vital to the human immune system including macrophages, dendritic cells and especially helper T cells (CD4 lymphocytes).2
HIV is spread through body fluids such as blood, semen, vaginal fluid, pre-ejaculate, or breast milk. Unprotected sexual contact is the most common means of transmission. Other means of transmission include blood transfusions, sharing of needles in IV drug use, and mother-to-child transmission in pregnancy, childbirth or breastfeeding.HIV infects the cells of the immune system and destroys them or makes them ineffective so that the immune system deteriorates and can no longer fight infection. Without antiretroviral treatment the disease typically advances through several phases:
- First year: rapid and transient decline in the number of CD4 lymphocytes;
- Progression over anywhere from a few months to more than 10 years: CD4+ T cell numbers slowly decline to below a critical level and the immune system can no longer fight opportunistic infections;
- Final stage: Onset of full-blown AIDS (Acquired Immune Deficiency Syndrome), marked by infection with one or more HIV-associated opportunistic infections or cancers and ultimately death.
Diagnosis
People living with HIV infection often do not know they are infected,3 in part because there are often no symptoms after recent infection. Yet these people are very infectious and may unknowingly transmit the disease. That’s why many authorities recommend HIV testing during routine medical care for adults, adolescents, and pregnant women.3 With early diagnosis, people can help prevent transmission and begin antiretroviral treatment sooner. There is increasing evidence that when treatment begins sooner, quality of life is better, there is a lower risk of transmission, and there is less chance of developing AIDS.3
Diagnostic testing
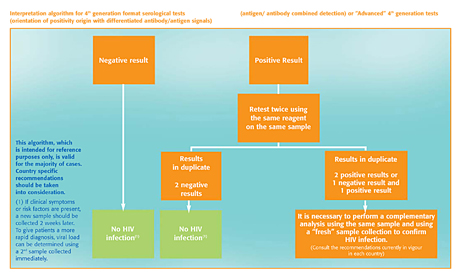
Conventional screening for HIV is usually first done through a blood sample, sputum or urine test to detect the presence of HIV antibodies.
- These tests are sensitive and accurate when antibodies are present in sufficient numbers, which is on average about 22 days after exposure.
- The use of combined “4th generation” ELISA (enzyme-linked immunosorbent assay) tests, which simultaneously detect HIV antibodies and the HIV1 p24 antigen, enable effective detection earlier than antibody-only tests.3
- Point-of-care rapid tests help make screening more accessible, so more people are tested earlier. This is particularly important in the developing world, where access to testing is an issue.
- When the result is positive, a confirmation is performed, often with an HIV-1 Western Blot or immunofluorescence assay.
Monitoring
- Quantitative molecular tests , such as PCR (polymerase chain reaction) or NASBA (nucleic acid sequence based amplification), are used to measure viral loads for people who are HIV-positive. It is important to regularly monitor viral loads to ensure effective antiretroviral treatment.4
- Use of a Dry Blood Spot (DBS) makes it easier to collect and transport blood samples for viral load monitoring. The simple filter paper format makes monitoring more accessible worldwide, particularly in remote areas.
Prevention / Treatment
Prevention
While there is currently no vaccine for HIV, preventing the spread of HIV infection is a key strategy of education and political campaigns aimed at eradicating the disease, including the 2011 United Nations Political Declaration on HIV and AIDS.5 Key prevention methods include:
- Reducing risk of sexual transmission with safe(r) sex:
- Reducing number of sexual partners
- Consistent use of condoms3
- Antiretroviral treatments help lower risk of spread in several ways:
- They reduce amount of virus in HIV-infected people, lowering risk of transmission, including mother-to-child6,7
- Treatment immediately post-exposure lowers the risk of contracting HIV8
- Oral pre-exposure prophylaxis (PrEP) is recommended for at-risk (focus: men and transgender women who have sex with men; serodiscordant heterosexual couples)9
- Regular screening of blood products and donor organs has reduced the risk of transmission during blood transfusions and organ transplantation to extremely low10
- Needle exchange programs for IV drug users help prevent transmission through shared needles11
Treatment
There is currently no cure for HIV or AIDS, but today’s antiretroviral drug treatments for HIV have greatly improved quality of life and prognosis for HIV-infected people.
- There are four classes of antiretroviral (ART) therapies
- Reverse transcriptase nucleoside inhibitors (RTNI)
- Non-nucleoside reverse transcriptase inhibitors (nRTNI)
- Entry and fusion inhibitors (FI)
- Protease inhibitors (PI)
- Treatment is optimized by using a combination of drugs from at least three of the four different classes of ARTs*.12 This may be called “triple therapy” or a “cocktail”.
- A key objective of treatment is to lower plasma viral load.
- CD4, viral load, and safety and metabolic state should be monitored.
- HIV-infected people should also receive immunizations and prophylaxis to help protect them from opportunistic infections.3
Guidelines
- World Health Organisation (WHO) Consolidated guidelines on the use of antiretrovirals for treating and preventing HIV infection
http://www.who.int/hiv/pub/guidelines/arv2013/en/ - World Health Organisation (WHO) Global update on HIV treatment 2013: results, impact and opportunities
http://www.who.int/hiv/pub/progressreports/update2013/en/ - UNAIDS Report on the Global AIDS Epidemic 2012
http://www.unaids.org/ - Screening for HIV: U.S. Preventive Services Task Force Recommendation Statement.
Virginia A. Moyer, MD, MPH, on behalf of the U.S. Preventive Services Task Force (USPSTF). Annals of Internal Medicine Clinical Guidelines: April 30, 2013
http://www.uspreventiveservicestaskforce.org/uspstf13/hiv/hivfinalrs.pdf - WHO recommendations on the diagnosis of HIV infection in infants and children
WHO: 2010. (NLM classification: WC 503.1)
http://whqlibdoc.who.int/publications/2010/9789241599085_eng.pdf - Guidelines for the prevention and treatment of opportunistic infections in HIV-infected adults and adolescents: recommendations from the Centers for Disease Control and Prevention, the National Institutes of Health, and the HIV Medicine Association of the Infectious Diseases Society of America. Panel on Opportunistic Infections in HIV-Infected Adults and Adolescents.
http://aidsinfo.nih.gov/contentfiles/lvguidelines/adult_oi.pdf
REFERENCES
- UNAIDS, WHO 2011
- Cunningham, A. et al. "Manipulation of dendritic cell function by viruses".Current opinion in microbiology 13 (4): 524–529. .
- Moyer, VA. Annals of Internal Medicine Clinical Guidelines: Screening for HIV: U.S. Preventive Services Task Force Recommendation Statement. April 30, 2013
- Dewar R, et al. Diagnosis of human immunodeficiency virus infection. In: Mandell GL, Bennett GE, Dolin R, eds. Principles and Practice of Infectious Diseases. 7th ed. Philadelphia, Pa: Elsevier Churchill Livingstone; 2009:chap 119.
- UNAIDS Report on the Global AIDS Epidemic 2012
- Cohen MS, et al. Prevention of HIV-1 infection with early antiretroviral therapy. The HPTN 052 Study Team.N Engl J Med 2011.
- WHO recommendations on the diagnosis of HIV infection in infants and children. WHO: 2010. (NLM classification: WC 503.1)
- CDC. Antiretroviral post-exposure prophylaxis after sexual, injection-drug use, or other non-occupational exposure to HIV in the United States: recommendations from the U.S. Department of Health and Human Services. MMWR 2005;54(No. RR-2):1-20
- Guidance on oral pre-exposure prophylaxis (PrEP) for serodiscordant couples, men and transgender women who have sex with men at high risk of HIV: Recommendations for use in the context of demonstration projects. WHO: July 2012.
- Rogers MF, et al. National Center for Infectious Diseases Jones WK., Dr. P.H. Office of the Associate Director for HIV/AIDS. Guidelines for Preventing Transmission of Human Immunodeficiency Virus Through Transplantation of Human Tissue and Organs. CDC: May 20, 1994 / 43(RR-8);1-17
- Bruneau J, et al. Trends in Human Immunodeficiency Virus Incidence and Risk Behavior Among Injection Drug Users in Montreal, Canada: A 16-Year Longitudinal Study. Am. J. Epidemiol. (2011) 173 (9): 1049-1058.
- Guidelines for the Use of Antiretroviral Agents in HIV-1-Infected Adults and Adolescents. Panel on Antiretroviral Guidelines for Adults and Adolescents. Department of Health Services (http://www.aidsinfo.nih.gov/)
Az oldal tartalma nem tekinthető orvosi tanácsnak
Az oldal egészségügyi tartalma összefoglaló formában jelenik meg, jellegét tekintve általános, és csak tájékoztatásra szolgál. Az oldal szerzőinek nem állt szándékában és nem is ajánlatos a tartalmat professzionális orvosi tanács helyett használni. Az oldal egészségügyi tartalmát nem szabad egészségügyi vagy közérzeti probléma vagy betegség diagnosztizálására használni. Mindig kérjen tanácsot orvosától vagy más egészségügyi szakembertől bármilyen egészségügyi problémával vagy kezeléssel kapcsolatban. Az oldal semmilyen tartalmát sem szánták orvosi diagnózisnak vagy kezelésnek. Orvosok nem használhatják fel egyedüli forrásként a felírandó gyógyszert érintő döntésekhez. Soha ne hagyja figyelmen kívül az orvosi tanácsot, illetve ne halogassa, hogy orvoshoz menjen olyasmi miatt, amit ezen az oldalon olvasott.